There has been little change or improvement, say two local physiotherapists, in the year since they asked a government committee to support their efforts to bring more students north.
On Tuesday Hilary Crowley and Terry Fedorkiw gave the same dire presentation and offered the same solution: a plea for 20 more student seats at the University of British Columbia, but based in Prince George.
"Our situation is still critical," Crowley told the standing committee on finance at its Prince George meeting Tuesday evening, before asking for the group of MLAs to again support the recommendation for funding. "Nothing has changed since our (2015) presentation as far as our communities are concerned."
This year, Fedorkiw and Crowley created Physiotherapists for Northern Communities to ramp up their lobbying efforts, calling on the Ministry of Advanced Education to agree to expand UBC's annual intake from 80 students to 100, and assign those extra seats to the northern rural cohort to double the spots to 40.
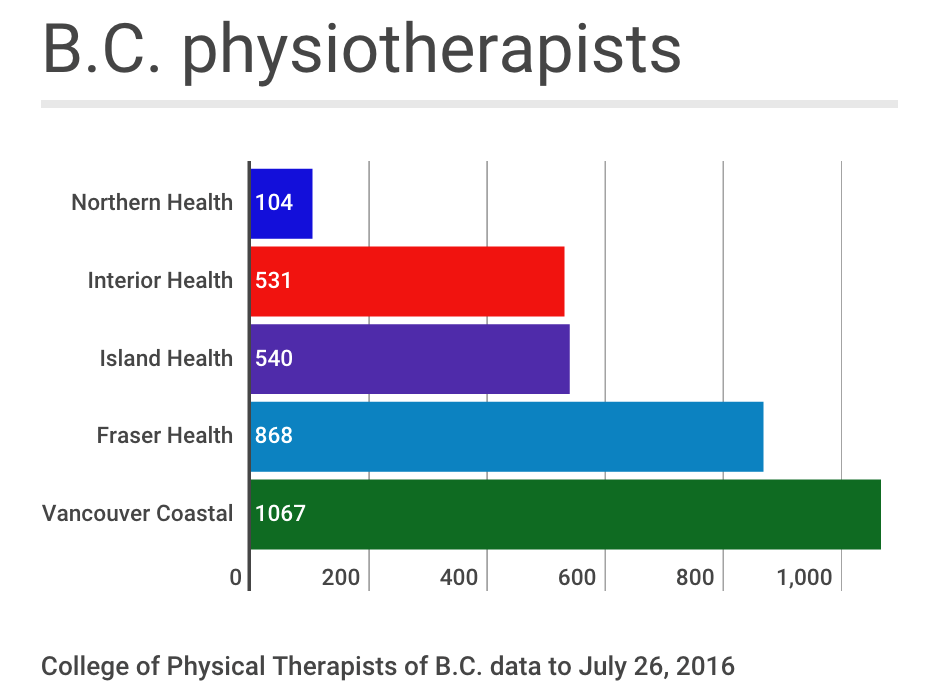
In August, The Citizen reported there are 104 registered physiotherapists, or about 3.3 per cent of the province's physiotherapists, working in the Northern Health region, despite it making up about seven per cent of B.C.'s population. Nine towns don't have publicly funded physiotherapy and more have unfilled positions. B.C. also lags behind other provinces in university spaces for training, with 80 offered at UBC, compared to 315 spaces at five Ontario universities and 262 at four Quebec universities. Alberta, with about 500,000 fewer people than B.C., has 110 training spots.

"We really don't understand why the government hasn't yet released the necessary funds to enable this program to come to fruition," said Crowley, adding the cohort is better at attracting young professionals into rural or remote settings.
"Training in Vancouver only causes more students to move away from northern and rural areas, whereas having the program at UNBC would enable the students to live in these communities and form bonds and networks, which would enhance their professional careers and encourage them to stay in the north where they are most needed."
Communities across the region are already feeling the impact of missing services. In Prince George, it's the temporary closure of the outpatient department due to staff shortages.
That means after orthopedic surgeries - especially knee and shoulder replacements - patients can't complete their rehabilitation at the hospital.
"It also makes it more difficult to discharge patients with stroke or chronic medical conditions, as these rehabilitation services aren't available to enable patients to return to their own home," said Fedorkiw, adding service to First Nations are "severely compromised by the shortage of available staff."
It should be reinstated - "hopefully" said Fedorkiw - in November.
Both said the call for spots has widespread support from doctors in the Northern Medical Society, local MLAs and city councils, and both the University of British Columbia and University of Northern B.C.
Doctors have stopped referring because they know the service isn't available but that data doesn't get tracked, Fedorkiw said, to give a true picture of the need for services.
"This means that patients are more likely to become dependent on medications and will have more frequent visits to their doctors or emergency departments. Physiotherapy is much more effective and less costly than these alternatives," Fedorkiw said.
Age is exacerbating the problem, Crowley said.. About 30 per cent of B.C. physiotherapists are over 50 and 10 per cent are over 60 years old.
"You can tell by looking at us," Crowley said. "We're now another year older than when we presented last year - and several of us are just hanging on in order to provide the necessary clinical teaching to the students."



