Karen Serwatkewich calls herself a long hauler and that has nothing to do with driving a semi-trailer.
For a while there, she felt like she’d been hit by a truck when her mind and body were being attacked by the COVID-19 virus.
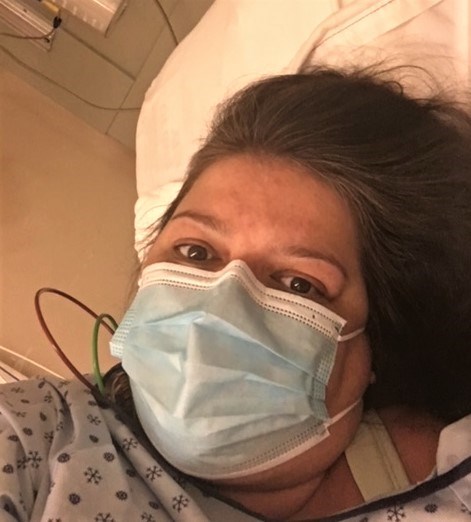
The 49-year-old Prince George woman was one of the first in the Northern Health region to be diagnosed with COVID and the lingering effects of the disease continue.
“I’m about 85 per cent better but I’m still dealing with brain fog and all those fun things that come with it,” said Serwatkewich.
Diagnosed on March 18, it started with pain in the back of her throat and a cough, followed by fever, fatigue and diarrhrea. Anxiety led to severe headaches, chest pain and numbness. Already dealing with sarcoidosis, a disease that causes inflammation, especially in the lungs, Serwatkewich made five trips to the emergency ward at UHNBC after she was diagnosed with the virus, each time struggling to breathe. Twice in late-March she had to call an ambulance. Her breathing had become so difficult and she was worried it was threatening her life.
“The fatigue was the worst, I couldn’t even walk to the bathroom a couple times, my fiancé had to help me,” said Serwatkewich. “It was two or three weeks where I was really fatigued and couldn’t breathe and I pretty much laid on the couch for quite a while. I never got headaches before.
“Your oxygen gets so low and anxiety kicks in and it was just one thing after another, it was horrible. I had bad bowel movements all the time; I actually wore Depends for over a month because I had no control. It wasn’t fun.”
In late-May she was admitted to hospital for five days with pneumonia. On June 5 her COVID test came back negative, but she still was not feeling well. The virus affected her skin and she lost about a third of her hair, which is just now starting to grow back. She’s an avid golfer who would shoot 36 holes per day several times a week her sickness kept off the course the entire year.
“The body aches and everything like that didn’t come until I got out of the hospital,” Serwatkewich said. “I was laying there and woke up and almost every part of my body and my bones started cracking, it was the weirdest thing. It was cracking everywhere and I started getting really bad pain, mainly in the shoulder and neck. It just seems like it goes through your entire body.”
She was taking prescribed morphine tablets to relieve her pain and prednisone to suppress her immune system and help clear her lungs but she’s pretty much stopped taking those drugs and replaced them with natural supplements, magnesium and vitamins C and D.
It wasn’t until November that Serwatkewich started to feel able to function again. She still hasn’t felt healthy enough to return to her full-time job as a manager/server at the Carmel Restaurant and Bon Voyage Inn but is working part-time at home as an accountant handling payroll and taxes for the two businesses.
Serwatkewich has discovered a Facebook page for COVID survivors – COVID Long Haulers Support Group Canada - which allows to people to share their personal stories and what they’ve gone through and continue to deal with as they recover from the effects of the killer virus. The long haulers page was started by Susie Goulding in Oakville, Ont., and when Serwatkewich joined in June there were 300 members. It now has 12,000.
“It’s helped me so much,” she said. “When I wasn’t getting better I thought I was the only one and I was like, why me? My fiancé (Eric Liimataminen) got sick but that was like six days and it was minor and he got over it.
“Because the stress level I had, I was so depressed and crying quite a bit, but to find this group and knowing that people are actually going through this, it took the stress level down eight notches. I can communicate with people and they know what I’m going through. I didn’t have to be alone through it.”
COVID was a new disease when Serwatkewich first got sick and at that time not much was known in the medical community about how to treat it. Doctors have since learned how to recognize warning signs to look for before people become severely ill and in many cases their interventions prevented patients from having to be put on breathing tubes. Now a year into the pandemic, the medical community continues to discover new ways the virus is damaging human health while they also try to develop better forms of treatment.
“There’s tons of us out there that have lingering effects and it seems it goes it in spurts what happens to you,” she said. “Two or three months ago I had twitching all through my body all the time and sometimes it hurt, like the twitches were trying to break through my skin.
“I still get brain fog and my feet really hurt. I have to take lots of pills to get myself to sleep.”
Serwatkewich says there’s a need for clinic in Prince George to help people deal with the physical symptoms and emotional stress of being a COVID long hauler and the help alleviate the costs of medication and massage therapists. For her, the closest COVID clinics are a day’s drive away in Vancouver or Edmonton.
“There’s three in Vancouver, we’re the northern capital of B.C. and there’s nothing here,” she said. “They get researched and studied and get rehab, and I know my doctor would refer me to it but then it would cost money to go down there. Quite a few people in Prince George (who had COVID) haven’t returned to their jobs completely and if we had a clinic with a group of doctors that can help us get back to somewhat normal, it would help a lot of people.”