Babies born prematurely in Prince George now have better access to breast milk with the creation of a milk donation site at the University Hospital of Northern BC.
The depot opened quietly in July, but was part of a province-wide announcement Tuesday of six new locations. Now BC Women's Hospital is calling on local women to consider donating their milk.
"I am thrilled that we've finally gotten to the point where all the NICUs (neonatal intensive care unit) in the province will have the same standard of care, which is using pasteurized donor's milk in the absence of the mother's own," said Frances Jones, who has run the provincial milk bank, located at BC Women's, for the last 16 years. "I'm hoping that we will have so much milk flowing forth that we will be able to actually offer it in the maternity units in the province."
In 2013, the province gave a $650,000 grant to the hospital in part because "research (shows) babies in neonatal intensive care units receiving breast milk have shorter stays in hospital, fewer infections and few hospital readmissions in the first year of life."
It's part of an ongoing push to increase access to breast milk.
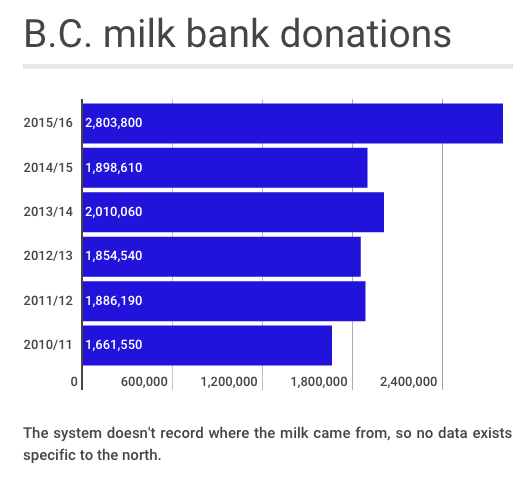
Last year donations jumped by almost 50 per cent after it opened 17 depots in the Lower Mainland through a partnership with Fraser Health in 2014. That added 500,000 millilitres of the 2,803,800 mL donated to to the B.C. bank last year.
But there still isn't enough for all of B.C.'s babies in need.
Over the years Jeanne Hagreen has packed bags of frozen milk from northern mothers who wanted to contribute and taken them with her on flights to Vancouver.
She remembers the looks she'd get dropping off the cooler box with large letters saying 'Do not thaw.'
Now there's no need for that extra effort.
"It just brings a smile to your face because this is something we've wanted for so long," said Hagreen, who retired from her position of 20 years as a lactation consultant at UHNBC last September after serving a total of 38 years on the maternity ward and has been a longtime advocate for the service.
Human milk is very important for premature infants, Jones said. It reduces the risk babies will get necrotizing enterocolitis (NEC) - a disease of the bowel.
"Babies that are born premature, because their systems are less developed, are at much higher risk to develop NEC and if we feed them formula they're at - depending on what study you read - somewhere between three and 10 times more likely to develop it," Jones said.
"We know by having pasteurized donor milk we can reduce the incidents and just have healthier babies."
It's taken the last three years to set up agreements with all of the health authorities.
Northern donors must first be screened by the provincial bank and will drop off frozen milk at UHNBC where it will be shipped to Vancouver to be screened, pasteurized and redistributed across the province. For the first six months, BC Women's will pay to ship milk from Northern Health to BC Women's and then for the processed milk back to Northern Health. After that Northern Health will take on the shipping costs.
Northern Health did not provide comment by deadline on Tuesday.
"Donors understand that some of the babies are very fragile and won't make it without human milk," Jones said.
"It really is an amazing gift."
Workers at the Prince George and District Elizabeth Fry Society, which offers support programs for new mothers, see a need for the services among the mothers they serve. They echo Jones' hope that the milk bank could be expanded beyond the neonatal units especially for women who don't have the option of breastfeeding their babies.
"There's sexual abuse and body image issues and society issues that make breastfeeding difficult," said Jodie Flanagan, family support worker. "There's all this information out there about breastfeeding and how good it is for your baby but it's the accessibility and the availability that is the struggle."
Between 80 and 90 per cent of the mothers they work with breastfeed immediately after birth, but at six months that number drops to 50 to 60 per cent.
Flanagan and resource nurse Jody Youb call breast milk a baby's first vaccination.
"It decreases diseases and infections and tons of other things," said Youb, adding that early start could have a positive snowball effect on the healthcare system.
"A lot of our moms do come from a poverty background and giving the baby that good start to good health is better in the long run," Flanagan said.
For those interested in becoming a donor, visit www.bcwomens.ca/donate or call 604-875-2424, local 6013 for more information.



